Abstract
Sickle cell disease (SCD) is an inherited blood disorder that affects 100,000 persons in the US. Despite affecting a small percentage of the US population, health care costs for SCD are approximately 1.7 million for total lifetime cost mostly due to high healthcare utilization. Though outpatient comprehensive SCD centers reduce healthcare costs by decreasing acute visits, there has been little in the literature on optimizing inpatient SCD care and facilitating a successful transition back to outpatient care. Improving the transition between inpatient care and the outpatient provider may also reduce health care expenses. Current inpatient models of care for adults with SCD vary among hospital centers, but are generally a combination of hematology and oncology providers, internists, and/or SCD specialists. Similar to most hospital systems, our internal medicine resident teams and hospitalists provide most of the care for adults with SCD. The hematology consult team is only consulted for a small number of adults with SCD who have severe complications due to limited capacity.
Prior to 2020, the discharge planning, transfusion guidance, and pain management for adults with SCD in the hospital was highly variable. To improve continuity of care, we developed a new inpatient model of care using electronic communication (e-consult) notes that encompass the important aspects of management (i.e. individualized care plan, etc.) for every patient admitted with SCD. At the time of admission, the SCD team receives an EMR-alert to initiate the consultation and does not require an order from the inpatient team. This inpatient model of care was also helpful during the COVID-19 pandemic when the hospital experienced a shortage of staff making it more difficult for the hematology consult services to participate in SCD care. We hypothesized that the e-consult service would increase the inpatient medical teams’ satisfaction level with care and improve discharge planning for adults admitted with SCD.
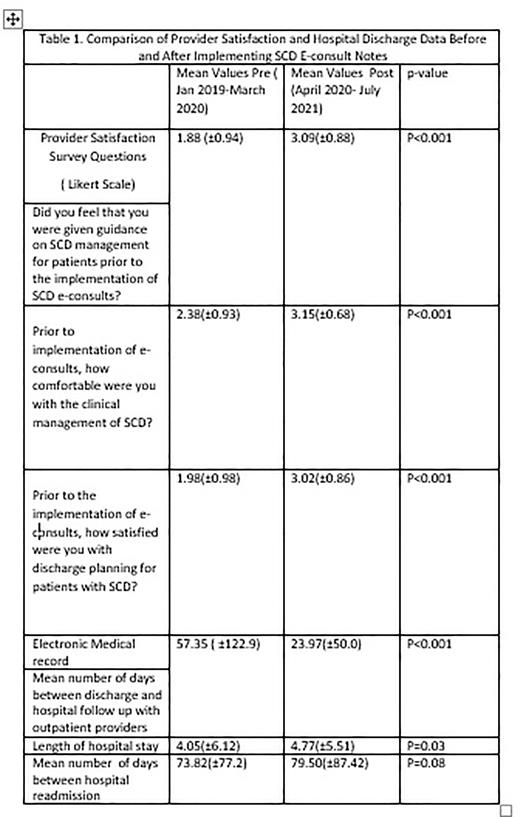
Methods: We analyzed 1,282 inpatient visits during January 2019 to July 2021. The e-consult notes, written by a SCD specialist, provided recommendations on the following: electronic medical record review (hospital course, vital signs, and laboratories), outpatient treatment plans, best-practices from the national SCD guidelines, and discharge planning. E-consult notes were written beginning in April 2020. Inpatient provider teams were asked to complete surveys measuring satisfaction of the SCD management before (Jan 2019-Mar 2020) and after (Apr 2020-Jul 2021) the implementation of e-consults. Time to first discharge appointment, length of stay, and hospital readmission were obtained using the electronic medical record. We used ANOVA test to compare mean values between the two time periods.
Results: There were a total of 106 providers who participated in the satisfaction survey, but three entries were incomplete. The majority of inpatient provider teams who responded were internal medicine (76%; 80/106). Only 61% (62/103) of the providers were familiar with the e-consult service. Among those familiar with the e-consult service, 79.6% (45/62) of the providers followed the recommendations of the e-consult service. Over 80% of the providers reported that e-consults were valuable to SCD care, promoted good quality of care, and resulted in an overall improvement in the care of SCD. Furthermore, provider satisfaction were significantly improved. The mean number of days between hospital discharge and outpatient follow up were also significantly lower than before the implementation of this service. The length of hospital stay was statistically higher for the post implementation period, however remained under the national average of hospitalizations for SCD. The hospital readmission rate was unchanged.
Limitations: We are unable to capture hospital follow up that occurred at another institution due to patients being under another provider's care.
Conclusion: Improving inpatient care for people with SCD is important. Due to insufficient SCD staff, new models of inpatient care are needed. The e-consult program initiated at UAB can significantly improve inpatient team satisfaction, inpatient SCD guidance, and facilitate timely discharge with an outpatient SCD provider. E-consult notes can be an acceptable tool to help optimize inpatient care when a formal inpatient SCD service does not exist due to limited SCD staff.
Disclosures
Ogunsile:Forma: Honoraria; Clearview: Consultancy, Honoraria; Novartis: Consultancy, Honoraria; Global Blood Therapeutics: Consultancy, Honoraria; Guidepoint-Consultation Request: Consultancy, Honoraria; Vertex: Consultancy, Honoraria. Kanter:Novartis: Consultancy, Honoraria; University of Alabama Birmingham: Current Employment; Forma: Consultancy, Membership on an entity's Board of Directors or advisory committees; Fulcrum Tx: Consultancy; GLG: Consultancy; Ecor1: Honoraria; Guidepoint Global: Honoraria; Beam: Honoraria; Graphite Bio: Consultancy; ORIC: Consultancy; Bausch: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal